Cardioversion
If your heart has an irregular (uneven) beat or is beating too fast, cardioversion is a way to restore a regular rhythm.
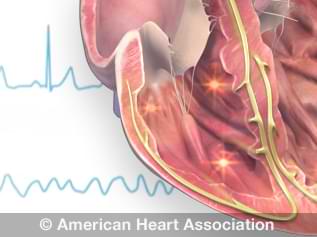
Watch an animation of arrhythmias.
There are two kinds of cardioversion. Your doctor may give you one or more medications to bring back your regular heartbeat. This is called pharmacologic (chemical) cardioversion. Doctors also restore regular rhythms by sending an electrical shock to the heart. This is called electrical cardioversion.
Why do people have cardioversion?
People have non-emergency or elective cardioversion to treat arrhythmias. The electrical signals that control your heartbeat start in the upper right chamber of your heart (atrium). In atrial fibrillation, very fast, irregular electrical signals move through both upper chambers of your heart. This can make your heartbeat fast and irregular. Some people who have atrial fibrillation don’t notice any changes in the way they feel. But others feel:
- Very tired
- Heart palpitations
- Short of breath
- Dizzy or faint
Cardioversion also treats other kinds of abnormal heartbeats, including atrial flutter, atrial tachycardia and ventricular tachycardia.
Cardioversion or defibrillation is also used in emergency situations for people who suffer sudden life-threatening arrhythmias.
What are the risks?
If you have atrial fibrillation, blood clots can form in your heart’s left atrium. Cardioversion may knock loose a blood clot in your left atrium. If the clot travels to your brain, it can cause a stroke. To avoid this, your doctor may give you medicine (such as warfarin) to make your blood less likely to form blood clots. If your doctor gives you the medication, you may need to take it for three to four weeks before the procedure. Transesophageal echocardiography (TEE) is often used to check for the presence of blood clots before this procedure.
Complications are uncommon but may include:
- Allergic reactions to the medications
- Irritation of the skin on your chest or back where the electrodes were applied during electrical cardioversion
- The potential for new or worsened arrhythmia that will need to be treated with medications, a pacemaker or an implantable cardioverter defibrillator (ICD)
How do I prepare for electrical cardioversion?
- Have someone drive you to your appointment and take you home. Arrange your schedule so you don’t have to drive, operate machinery or make any important decisions for the rest of the day after your cardioversion. Don’t eat or drink for at least eight hours before your procedure.
- Unless your health care professional has told you not to, take your usual medicines on the morning of your cardioversion. Bring a list of all your medicines (including over-the-counter medicines, herbs and vitamins) to your appointment.
- Leave all your jewelry at home.
- If you are having an electrical cardioversion, don’t put any lotions, powders or ointments on your chest and back for 24 hours before the procedure. They can cause problems with the paddles used to deliver electricity to your heart.
- You may be given blood-thinning medications before the procedure to prevent blood clots.
What happens during the procedure?
Your health care team can perform cardioversion in a hospital or clinic. If medications bring back your normal rhythm, you may not need electrical cardioversion. If you need electrical cardioversion, it may be done right away or scheduled for another day.
During an electrical cardioversion:
- Your nurse or doctor will place an IV in your arm and give you medication (sedative) to make you sleepy. You won’t feel pain during the procedure.
- Your doctor will deliver an electrical shock through two electrodes, one on your right chest, the other on the left ribs. Alternatively, one electrode may be placed on your chest and the other on your back, or both can be placed on your chest. The shock briefly stops (resets) your heart rhythm.
- Your doctor will check to see if your heartbeat is regular. Some people need only one shock. Some need more to restore a regular heartbeat.
What happens after cardioversion?
You can usually go back to your normal activities soon after cardioversion, using only medications.
After electrical cardioversion:
- You will be monitored carefully for an hour or more after the procedure.
- If appropriate, you can visit with family members right away, but you may feel sleepy for several hours.
- Your health care professional will tell you if the cardioversion worked and whether you need more treatment or need to take medication to maintain a normal heart rhythm.
- You can usually go home on the day of your procedure.
What happens after I get home?
Before you leave, you’ll get instructions about what to do at home. For a few days after electrical cardioversion, the skin on your chest and back may be irritated where the electrodes were placed. Ask your doctor about creams or medications that can help.